Short staffing in primary care is when the service doesn’t have enough staff with the right skills to provide patients with safe care and support. There are lots of things that can impact staffing levels and affect your service.
This article covers the contingency plans you should have in place to manage current and future workforce demands and maintain a safe, effective, and responsive service, even when unexpected absences occur.
The nursing workforce is critical in primary care and has the capacity to reduce adverse patient outcomes and contribute to the wider productivity of the primary care service. By utilising the skills of the nursing workforce, you can increase a patient's access to care, reduce the team's workloads, offer stability, continuity, and consistency, and help the practice reach the Quality Outcome Framework targets.
Here are five ways to deal with short staffing in a primary care environment:
- Understand the team's capabilities
- Effective rota system
- Reliable agency partner
- Succession plan in place
- Prioritise your workload
Primary care is the epitome of a multidisciplinary team, and you may have up to 30 types of professionals in your practice. Primary care is patient-centered and the distribution of roles amongst the teams may change according to patients' needs. Understanding the capabilities of your healthcare professionals is crucial when short staffing arises.
Utilise your healthcare assistants (HCAs) for health checks, blood samples, ECGs, and blood pressure checks to provide more capacity to the nursing team. Divide your nursing team by capability including competencies like diabetic, hypertension or asthma reviews, smear tests, contraception and chronic disease reviews and prescribing to provide more capacity for the GPs.
By reshuffling and utilising everyone’s skills and competencies, and working as a team, you will be in a much stronger position if you find yourself short-staffed.
A good rota system will help you plan your schedule, communicate it with your staff and give them appropriate notice which supports their work-life balance. Rota changes are inevitable, so make sure changes are communicated as early as possible and explain why the rota has changed.
If you use an electronic system, you may be able to trigger alerts and notifications. For paper-based systems, it’s important to have a robust process in place with clear responsibilities outlined for those who are involved in arranging the rota. Schedule regular staff training on the rota system you have in place and designate senior staff as escalation points in emergencies that are responsible for determining safe staffing levels.
With an effective rota system in place, you can deal with staff resignations, sickness, parental leave, family leave, or annual leave more efficiently.
Despite your best efforts to cover short staffing internally, there may be times you need to work with an agency to reduce the impact on patients. It’s important to partner with a reliable agency that can provide candidates but also strategically assess your situation and suggest the most cost-effective and long-term workforce solutions for your practice.
At GP World, we pride ourselves on our commitment to thoroughly understanding your department or service. We recognise that every team is unique, with its own set of challenges, goals, and dynamics. By gaining a comprehensive understanding of your needs and preferences, we ensure that the candidates we present aren't just capable they're the right match for your specific requirements.
We're not here to simply provide a service; we're here to build lasting partnerships and contribute to the success of your practice. So, when you choose GP World, you can trust that we'll go above and beyond to deliver results tailored to your unique needs.
If you’re looking for primary care professionals to support your practice and a reliable agency partner, request a call back from GP World today
Not all short staffing is because a healthcare professional is off work for the short term. Sometimes, your practice might be short-staffed due to resignations, retirement, parental leave, unplanned activities, the introduction of a new service or long-term absences.
To create a succession plan, you need to identify your practice challenges for the next 5 years and the critical positions which are needed to support business continuity. Consider your high-potential healthcare professionals and work with them to build the competencies, skills, and knowledge to support the next stages of their career development and prepare them to step into critical positions in the future.
Nursing top talent is a win-win because it supports the progression of your team and builds a valuable contingency plan most cost-effectively.
During periods of short staffing, some tasks may need to be postponed. It’s important to prioritise the practice’s workload, so that the teams can complete their delegated jobs and ensure patient care is the priority.
Urgent tasks are things where immediate action is required such as a medical emergency and important tasks are usually related to the overall mission.
The Eisenhower Matrix is a popular strategy for deciding how to prioritise tasks.
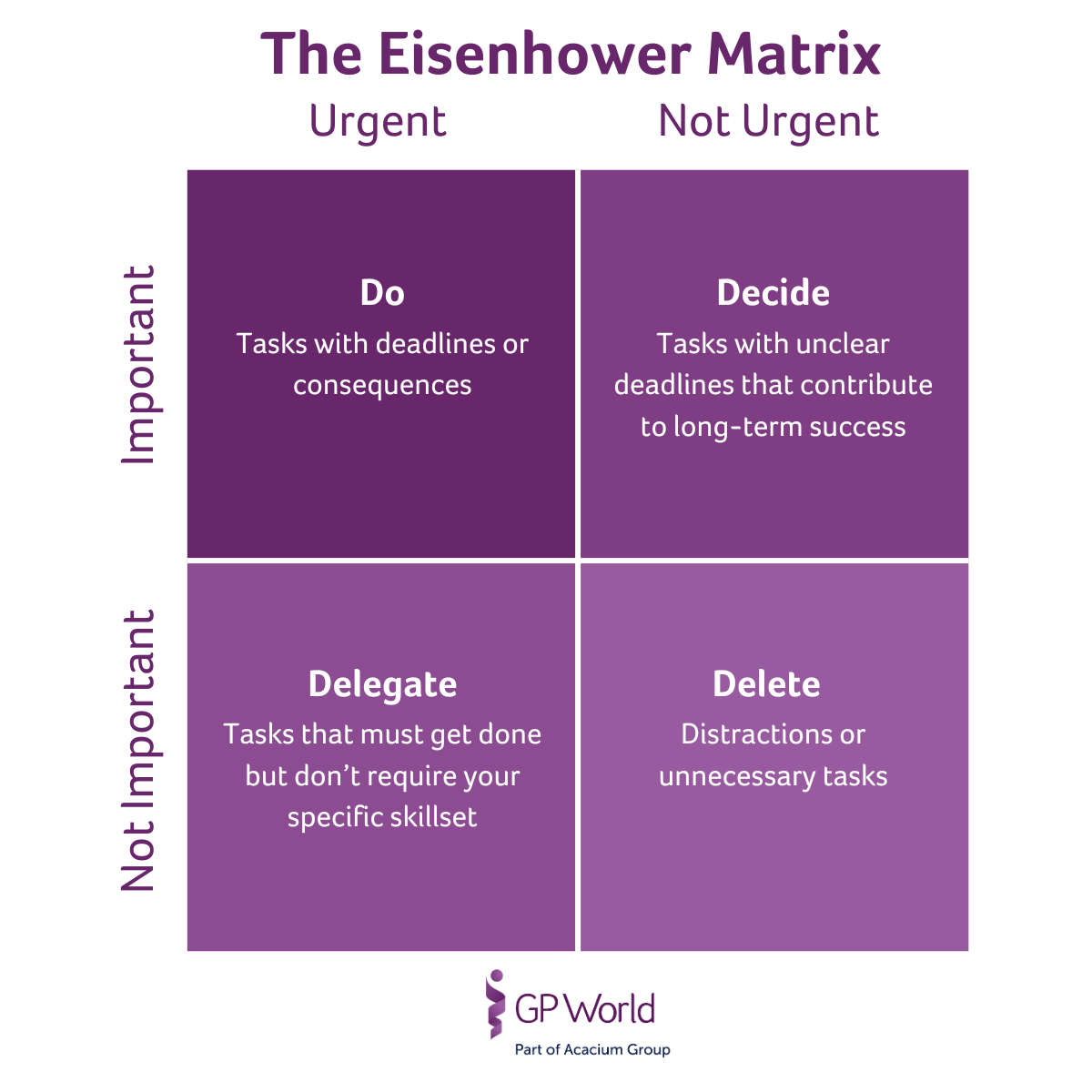
As you’ll have a succession plan in place and fully understand your team's capabilities, implementing the time management matrix should be an effective way to ensure staff with the right skills can provide patients with safe care and support.
Existing evidence on safe staffing levels is limited within primary care settings, as most research has taken place in acute hospital environments. The Royal College for Nursing recognised in their Staffing for Safe and Effective Care (2019) report that further research is needed in other settings.
The British Medical Association’s England GP Committee have generated a guide that enables practices to prioritise safe patient care. The average number of patients each GP is responsible for has increased by nearly 18% between 2015 and 2024. As a result, the average number of patients each full-time equivalent GP is responsible for now stands at 2,295.
The European Union of General Practitioners and BMA have recommended a safe level of patient contacts of no more than 25 contacts per day and GP. The number of required appointments for a GP practice varies depending on opening hours, the number of GPs and the size and structure of the wider team including roles like nurses, healthcare assistants, physiotherapists, and pharmacists. A widely accepted formula via NHS England by McKinsey (2008) suggests practices should offer 72 appointments for every 1,000 patients per week to meet the reasonable needs of their patients and provide them with access to safe care and support. With an ageing population, more complex healthcare issues and a backlog of patients, the formula could be considered outdated in the current healthcare climate and the demand GPs are facing in the UK, may be significantly higher.
By June 2023, the average number of patients per GP practice increased to 9,800. Based on the research and recommendations above, the average GP practice would need 5.6 FTE GPs to maintain safe staffing levels. The reality is that many practices are not able to meet recommended safe staffing levels with the demand they face, with a GP seeing an average of 37 patients per day (48% more than recommended). Clinicians have become responsible for providing extra capacity for patient care, despite the recommendations outlined. In the Care Quality Commission’s (CQC) Safe Staffing in General Practice, data was collected from a network of 37 practices to estimate the likely mix of attendances in primary care and reported morbidity problems. Health professionals interpreted the groups and estimated that:
- 37% of appointments needed a GP
- 63% could be delivered by other appropriately skilled members of the primary care workforce
The guidance on safe staffing levels in primary care requires more evidence, data and research. At this time, the consensus is that, based on the size of your practice, you need to have an appropriate number of staff across the primary care workforce with the right skills to provide patients with safe care and support.
Nurses play a vital role in healthcare systems, effectively preventing negative patient outcomes and improving overall system productivity. With round-the-clock high-risk clinical care, nursing significantly impacts patient wellbeing and has the capacity to reduce or avoid adverse patient outcomes.
GP World is a leading network of primary care professionals in the UK, providing qualified nurses, GPs and other primary care professionals to a variety of settings. Overcome your primary care staffing challenges and contact our dedicated team today.
Find qualified GPs and nurses today
We connect you with the best candidates from our database of over 5,000 GPs and nurse practitioners to solve your unique staffing needs. Our expertise is trusted by clients in the NHS, public and private sector across the UK.
Register a job